After the first coronavirus case was diagnosed in the United States in January 2020, the Trump Administration wasted two crucial months and failed to do mass testing to slow the spread of the virus. As a result, the coronavirus was able to spread undetected, rapidly tearing through communities across the country.
Now, more than two and a half months after the first confirmed case in the country, the U.S. is still struggling to test people who show symptoms of COVID-19. The US is only testing approximately 150,000 cases a day. Harvard Global Health Institute Director Dr. Ashish Jha has emphasized “That’s nowhere near enough,” explaining that such a low testing capacity has meant that in most states, people with mild symptoms are advised to self-quarantine at home rather than taking a test. Quest diagnostics, one of the largest commercial labs, still has a backlog of 80,000 tests for Covid-19.
Harvard’s Dr. Ashish Jha believes “Testing on this scale—about 500,000 people daily—is well within our capacity, and as the disease burden comes down, so will the number of tests we need to perform.” Conducting 500,000 tests a day will require the U.S. to invest in infrastructure like swabs, reagents, and PPE that doctors are experiencing shortages of.
Here’s why Trump’s failed leadership is to blame for the current shortages:
The United States Is Still Lagging Behind Other Countries On Testing
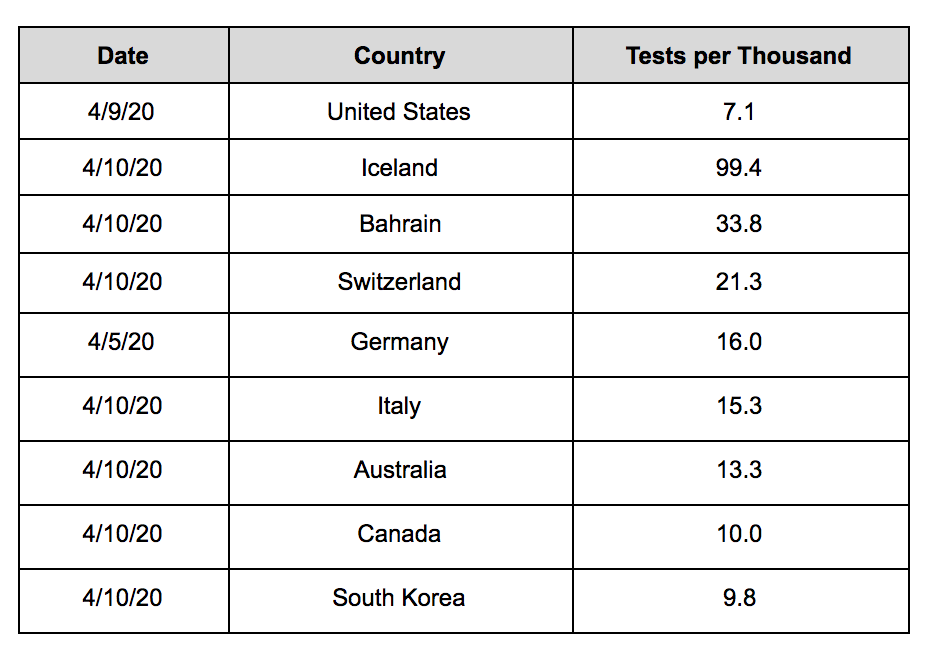
Data on COVID-19 testing collected by Our World in Data shows that the United States lags behind other countries on testing:
Five Reasons Why Donald Trump Is Still Struggling To Test Everyone Who Should Be Tested
Donald Trump would like the American people to think that anyone who needs to be tested for coronavirus has the option to do so, but the reality is that testing remains limited. Here’s a look at why that is:
#1: There Still Aren’t Enough Testing Kits.
-
Hospitals Have Been Unable To Keep Up With Testing Demands Because They Lack Complete Kits Or The Supplies Needed To Complete Tests. “Hospitals explained that they were unable to keep up with testing demands because they lacked complete kits and/or the individual components and supplies needed to complete tests, such as nasal swabs, viral transfer media, and reagents used to detect the virus. These shortages left hospitals unable to effectively test staff, patients, and others in the community who reported that they were concerned about possible exposure.” [HHS Office of Inspector General, April 2020]
-
Chief Executive Of UC Davis Health Dr. David Lubarsky: “Every Single Person Should Be Tested Who Presents With Symptoms That Suggests They Have Covid-19…But The Reason We Are Not Suggesting That Is The Lack Of Available Test Kits.” “At UC Davis Health in Sacramento, Dr. David Lubarsky, the health system’s chief executive, said the health system had a large testing instrument from Roche that could run more than 1,000 tests a day, but the company had been sending enough supplies to run only a few hundred tests per day. “Every single person should be tested who presents with symptoms that suggests they have Covid-19,” Dr. Lubarsky said. “But the reason we are not suggesting that is the lack of available test kits.” [New York Times, 4/6/20]
-
American Clinical Laboratory Association President Julie Khani: “We’re Hearing From Many Labs, And Not Just Members, That Shortages Of Test Kits Are Limiting The Ability To Continue To Build And Expand [Testing] Capacity.” “But further growth at these private labs, which the Trump administration has relied on to conduct widespread screening of Americans, may be a challenge. ‘We’re hearing from many labs, and not just members, that shortages of test kits are limiting the ability to continue to build and expand that capacity,’ ACLA President Julie Khani told POLITICO.” [Politico, 4/7/20]
#2: There Aren’t Enough Medical Supplies, Like Swabs, That Are Needed To Conduct Tests.
-
The New York Times Reported That Supplies Of Test Swabs Were So Low That Most Hospitals Tested Only Their Most Vulnerable Patients. “Supplies of test swabs have gotten so low that most hospitals test only their most vulnerable patients, typically those being admitted.” [New York Times, 4/6/20]
-
Harvard Professor Of Epidemiology Michael Mina Explained That The Biggest Problem For Hospitals In The Last Few Weeks Has Been A Global Shortage Of Swabs. “‘The biggest problem in the last couple of weeks has been how to get the 10-cent swab to put into somebody’s nose to get that sample out of somebody and into a test,’ Michael Mina, assistant professor of epidemiology at Harvard T.H Chan School of Public Health, said during a webcast Tuesday. ‘That’s something that hospitals across the globe are really trying to problem-solve around at the moment.’” [Wall Street Journal, 4/5/20]
-
A California Emergency Room Doctor Explained That Her Hospital Had So Few Test Swabs That Doctors Were Only Allowed To Use Them For Patients Who Were Admitted, Over 65 With Medical Problems, Or Pregnant. “At another hospital in California, an emergency room doctor, who asked not to be named for fear of losing her job, said she had to send home a patient who most likely had a bad case of Covid-19. The hospital has so few test swabs that doctors are permitted to use them only for patients who are admitted, who are over 65 with diabetes or other medical problems, or who are pregnant. Reluctantly, the doctor sent her home, with a face mask and instructions on hand-washing, which can provide only limited protection in her tight, multifamily living quarters.” [New York Times, 4/6/20]
-
There Are Shortages Of The Chemical Mixture That Accompanies The Testing Swab To Preserve Genetic Material In The Sample. “Another scarce resource is the viral transport media, the chemical mixture that accompanies the swab and preserves genetic material in the sample. Many institutions and labs are starting to make it themselves, sometimes using materials and expertise from closed research labs. On March 21, the Centers for Disease Control and Prevention posted a do-it-yourself recipe for the product online.” [Wall Street Journal, 4/5/20]
-
Labs At Places Such As New York University And Stanford Have Started To Make Their Own Chemical Mixtures To Conduct Tests Because They Have Not Been Able To Buy Enough. “Labs at places such as New York University and Stanford University are starting to make their own chemical mixtures because they can’t buy enough. A high-school lab in Tennessee managed to set up testing operations, with two science teachers leading the charge to reduce turnaround time in their area. And Northwell Health, a hospital network in New York, said it is making its own 3-D printed swabs to take samples from patients’ throats or noses.” [Wall Street Journal, 4/5/20]
-
Professor Of Laboratory Medicine At University Of California, San Francisco Steve Miller: “Doing Any Testing Requires Four Things: Space, Staff, Instrumentation, Reagents… All Four Of Those Have Had To Be Dealt With And Expanded.” “Doing any testing requires four things: space, staff, instrumentation, reagents,” said Steve Miller, a professor of laboratory medicine at the University of California, San Francisco. “We found that all four of those have had to be dealt with and expanded.” [Wall Street Journal, 4/5/20]
#3: Because The Trump Administration’s Early Testing Failures Allowed The Virus To Spread Undetected For So Long, Demand For Testing Has Skyrocketed, Overwhelming The System.
-
Because The Virus Spread Rapidly, The New York Times Reported That Demand For Testing Has Overwhelmed Many Labs And Testing Sites. “More and more rapid tests are coming onto the market and private companies like Quest and LabCorp are now running thousands of tests a day. But as the virus has spread from state to state infecting hundreds of thousands of Americans, demand for testing has overwhelmed many labs and testing sites.” [New York Times, 4/6/20]
-
One Hospital Administrator Said: “Millions [Of Tests] Are Needed, And We Only Have Hundreds.” “One hospital administrator said that across the industry, ‘millions [of tests] are needed, and we only have hundreds.’ Without access to needed testing materials, some hospitals described dividing the media in COVID-19 kits in half to double their capacity and resorting to using the transfer media in flu and strep kits to provide testing.” [HHS Office of Inspector General, April 2020]
-
Given Low Testing Supplies, Hospitals Prioritized Testing Their Employees And Patients With More Severe Symptoms, Meaning Hospitals Were Not Able To Conduct Widespread Testing Of Patients And Community Members. “Given supply shortages and uncertainty about future access, hospitals reported prioritizing testing for their employees and for patients with more severe symptoms. Prioritized testing meant that many hospitals reported they were currently unable to conduct widespread testing of patients and community members to help contain the spread of COVID-19.” [HHS Office of Inspector General, April 2020]
#4: Labs Are Overwhelmed And Still Processing Testing Backlogs, Contributing To Significant Delays In Testing Results.
-
Politico: “Labs Nationwide Are Overwhelmed By Patient Samples Flooding In As They Continue To Face A Shortage Of Critical Supplies. “Labs nationwide are overwhelmed by patient samples flooding in as they continue to face a shortage of critical supplies. A rapid test described by Trump in mid-March as a ‘game changer’ that would soon be available in doctors offices is still hard to come by for many Americans.” [Politico, 4/7/20]
-
Hospitals Described Extended Waits For COVID-19 Test Results, Reporting Frequently Waiting 7 Days Or Longer When Typical Turnaround For Virus Testing Is 24 Hours. “Hospitals described extended waits for COVID-19 test results. Hospitals reported frequently waiting 7 days or longer for test results. According to one hospital, 24 hours would typically be considered a long turnaround time for virus testing. Hospitals’ reliance on external laboratories contributed to delays, particularly as these laboratories became overwhelmed with tests to process from around the State or country. Hospitals also reported delays related to infrequent specimen pickups, mailing delays, and labs’ restrictive business hours. Some hospitals described success getting results more quickly by using commercial labs, whereas others received more timely results from public sources. Still others experienced inconsistent turnaround times, leaving them unable to predict when results would arrive or advise patients on how long they should self-quarantine or undertake other measures while awaiting results.“ [HHS Office of Inspector General, April 2020]
-
Quest Diagnostics, One Of The Largest Commercial Labs, Still Has A Backlog Of 80,000 COVID-19 Tests. “In early March, the nation’s two largest commercial labs, Quest Diagnostics and LabCorp, started testing, and they have acknowledged that their labs around the country were overwhelmed. Quest’s backlog is 80,000, according to the company, down from 160,000 on March 25. LabCorp says it has caught up, and now has a turnaround of four to five days from pickup.” [New York Times, 4/6/20]
-
The Rapid Test, Which Could Help Reduce Testing Delays And Increase Testing Capacity, Remains Unavailable To Most States — Abbott Had Only Sent Tests To Customers In 21 States As Of April 3. “Even that is not enough to meet demand from the IHS and state public health labs. “So far, the rapid test has not been available to us and there’s no chance of us getting it anytime soon,” Michael Kilkenny, executive director of the Cabell-Huntington Health Department in West Virginia, told POLITICO. The company said it sent supplies for 190,000 rapid tests to customers in 21 states as of last Friday. Abbott plans to expand production from 50,000 tests per day to about 65,000 by June. Other companies, including Cepheid, are manufacturing their own rapid tests.” [Politico, 4/7/20]
#5: The Trump Administration Has Long Been Antagonistic Toward Testing And Is Continuing To Shift Resources Away From Testing.
-
The Trump Administration Has Already Decided To End Funding For Some Local Coronavirus Testing Sites. According to NPR, “Some local officials are disappointed the federal government will end funding for coronavirus testing sites this Friday. In a few places those sites will close as a result. This as criticism continues that not enough testing is available. In the Philadelphia suburbs, Montgomery County has a drive-through site that has tested 250 people a day since March 21.” [NPR, 4/8/20]
-
Contradicting Experts, Trump Said He Did Not Believe The United States Needed Mass Testing Before Reopening The Economy. REPORTER: “Yeah, Mr. President, how could the administration discuss the possibility of reopening the country when the administration does not have an adequate nationwide testing system for this virus? Don’t you need a nationwide testing system — ” TRUMP: “No.” REPORTER: “ — for the virus before you reopen the economy?” TRUMP: No. We have a great testing system. We have the best — right now, the best testing system in the world.” [White House Press Conference, Washington, DC, 4/9/20]
-
In March, Trump Said He Wanted To Keep Grand Princess Cruise Passengers Who Tested Positive For Coronavirus On The Ship Because He Liked The Testing Numbers Being Where They Were. Trump discussed the Grand Princess cruise passengers during a March 6, 2020 briefing at the CDC: “I have great experts, including our Vice President, who is working 24 hours a day on this stuff. They would like to have the people come off. I’d rather have the people stay, but I’d go with them. I told them to make the final decision. I would rather — because I like the numbers being where they are.” [Press Conference, Atlanta, GA, 3/6/20]


